A beginner’s guide to Inflammatory Bowel Diseases (IBD)
Published by HUB Organoids on Feb 26, 2024
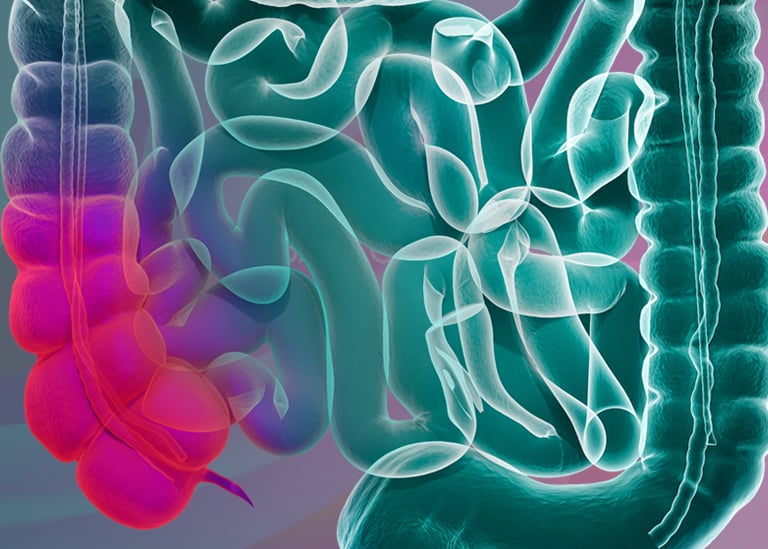
Inflammatory Bowel Disease (IBD) is a complex condition that affects millions worldwide. Understanding its nuances is crucial for patients, caregivers, and those seeking to enhance their knowledge of gastrointestinal health. In this beginner's guide, we'll delve into the basics of IBD, its potential causes, and available treatment options.
Defining IBD
IBD encompasses two primary conditions: Crohn’s disease (CD) and Ulcerative colitis (UC). These conditions provoke chronic inflammation and damage within the gastrointestinal tract, impairing its normal functions.
| Ulcerative Colitis | Crohn’s disease |
|---|---|
| Inflammation is usually only in the colon | Inflammation anywhere in the digestive tract |
| Continuous inflammation, not patchy | Inflammation in one or more patches |
| The colon wall is thinner and shows continuous inflammation | The bowel wall is thickened with a cobblestoned appearance due to patchy inflammation |
| Granulomas not present | Granulomas often present |
Despite the differences, both UC and CD share many similarities in symptoms which include fatigue, weight loss, abdominal pain, persistent diarrhea, and rectal bleeding.
What causes IBD?
The exact cause of IBD remains elusive, but it's believed to stem from a complex interplay of genetic predisposition, immune system dysfunction, and environmental triggers.
Scientific studies highlight the significant role of genetics in IBD. Approximately 5-20% of individuals with IBD have a first-degree relative with the condition, indicating a familial predisposition. The risk of developing IBD is notably higher in children of affected parents, especially when both parents have IBD. However, genetic susceptibility alone doesn't guarantee the onset of the disease; it merely increases the likelihood. Multiple genes, including NOD2/CARD15, have been linked to IBD, with up to 20% of patients having mutations in this gene. While genetic testing can identify potential risk factors, it's not a standard diagnostic tool due to the complexity of disease development and the influence of environmental factors.
The specific environmental factors responsible for triggering IBD remain unidentified, although various potential risk factors have been explored. Further research is necessary to fully comprehend these risk factors. Noteworthy factors include:
- Smoking: Active smokers have a significantly higher risk of developing Crohn’s disease compared to nonsmokers. Surprisingly, the risk of ulcerative colitis is lower in current smokers compared to those who have never smoked. However, the detrimental health effects of smoking outweigh any potential benefits for individuals with ulcerative colitis.
- Antibiotics: There is evidence suggesting that antibiotic usage may elevate the risk of IBD.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs such as aspirin, ibuprofen, and naproxen may increase the likelihood of developing IBD and exacerbate symptoms.
- Appendicitis: Children who undergo an appendectomy are less likely to develop ulcerative colitis later in life but may face an increased risk of Crohn’s disease. However, the benefits of appendectomy for severe acute appendicitis generally outweigh the risks.
- Diet: While no single food triggers IBD, certain dietary factors can exacerbate symptoms in some individuals. Further research is necessary to fully understand the impact of diet on Crohn’s disease and ulcerative colitis.
Treatment options
There are five primary classes of medications utilized in the treatment of IBD:
- Aminosalicylates: These anti-inflammatory compounds, containing 5-aminosalicylic acid (5-ASA), such as sulfasalazine, balsalazide, mesalamine, and olsalazine, are administered orally or rectally. They work to reduce inflammation in the intestinal wall and are predominantly used to manage symptoms and sustain remission in ulcerative colitis, though they may not be as effective for Crohn’s disease.
- Corticosteroids: Including prednisone, prednisolone, and budesonide, corticosteroids regulate the body’s inflammatory response, keeping the immune system in check. They are effective for short-term management of flare-ups but are not recommended for prolonged use due to their side effects, which encompass infection susceptibility, bone loss, weight gain, cataracts, skin fragility, sleep disturbances, and mood swings.
- Immunomodulators: This category of medications alters immune system activity to prevent persistent inflammation. Examples include azathioprine, 6-mercaptopurine (6-MP), and methotrexate. They are typically employed to maintain remission in individuals who have not responded to other treatments or who have only responded to steroids. Another immunomodulator that is commonly used is the Janus kinase (JAK) inhibitor, tofacitinib. Tofacitinib acts by blocking the action of enzymes involved in inflammatory processes.
- Antibiotics: Ciprofloxacin and metronidazole offer limited benefit for individuals with Crohn’s disease affecting the colon or perianal area, particularly in cases of infections like abscesses. Antibiotics are not strongly supported by scientific evidence for the treatment of ulcerative colitis.
- Biologic therapies: These are the latest advancements in IBD treatment, reserved for individuals with moderately to severely active disease unresponsive to standard therapies. Four of these agents (adalimumab, certolizumab pegol, golimumab, and infliximab) target a pro-inflammatory protein called tumor necrosis factor (TNF), while natalizumab and vedolizumab function by inhibiting certain types of white blood cells from infiltrating inflamed tissues.
The new way forward for IBD therapies
Research indicates a rising prevalence of IBD globally, underscoring the need for ongoing research efforts. In 2017, 6.8 million cases of IBD were detected globally. The increasing prevalence and complex nature of inflammatory bowel disease (IBD) underscore the critical need for innovative therapeutic approaches. While existing medications such as aminosalicylates, corticosteroids, immunomodulators, antibiotics, and biologic therapies have improved outcomes for many patients, there remain significant challenges. Notably, a subset of patients fails to respond adequately to current treatments, experiencing persistent symptoms and disease progression. Moreover, long-term use of certain medications, such as corticosteroids, can lead to debilitating side effects, highlighting the need for safer alternatives.
High-quality preclinical studies are needed to ensure the efficacy and safety of IBD clinical studies. The main preclinical research models for IBD are animal models and cellular models. Historically, animal models have been favored due to their perceived superiority over cellular models, which often lack representativeness. However, animal models come with drawbacks such as lengthy experimental timelines, species differences from humans, high costs, and ethical considerations. Conversely, while 2D intestinal cell models offer simplicity and cost-effectiveness, they fall short in replicating the complex physiology of the human intestinal environment. Moreover, they tend to lose their differentiated phenotype over time and fail to develop integral intestinal epithelial structures. In contrast, 3D patient-derived organoids derived from patient tissue or biopsies present a promising alternative. Recent advancements in culture conditions enable the differentiation of intestinal stem cells into all intestinal cell types. Organoid cultures recapitulate the physiology of the human intestinal niche and are genetically stable over long-term cultures. Additionally, they can be co-cultured with stromal cells or microbiome components to investigate complex facets of IBD pathogenesis.
Conclusion
In conclusion, Inflammatory Bowel Disease (IBD) represents a significant global health challenge, affecting millions with its complex interplay of genetics, immune responses, and environmental factors. This beginner's guide has aimed to demystify the basics of IBD, shedding light on the conditions of Crohn's disease and Ulcerative colitis, exploring potential causes, and discussing the current landscape of treatment options. As we have seen, while significant strides have been made in managing IBD, from the use of aminosalicylates to the advent of biologic therapies, the quest for more effective and safer treatments continues. The exploration of new therapeutic approaches, such as 3D patient-derived organoids, highlights the innovative directions being pursued in research. These advancements promise not only to enhance our understanding of IBD but also to open doors to clinically-relevant and more effective treatments in the future. As we navigate this evolving field, it's crucial for researchers to stay informed and engaged in the ongoing dialogue around IBD, fostering a spirit of innovation with more patient-derived platforms for testing novel hypotheses.
Looking to incorporate patient-derived organoids into your IBD research? Click here to learn more about our services.


.jpg)