PDO Screen – Patient-derived Organoids meet Cancer Modeling
Published by HUB Organoids on Mar 21, 2023
Discover how patient-derived organoids can revolutionize oncology research by enabling accurate modeling of tumor biology and predicting patient response to treatment.
We have come a long way in treating cancer. From surgeries, radiations, and injecting systemic drugs, to tailoring therapies that delicately disintegrate tumors. Despite advances in the field, there is still a considerable distance to go. The current statistics indicate that 95% of the anti-cancer agents that are developed in the preclinical phase falter as they progress toward clinical trials.
The complexity of cancer biology
Let’s be real. Cancer is an excruciatingly complex disease.
Recent advances in genomics have demonstrated layers of genetic, transcriptomic, epigenetic, and /or phenotypic evidence that could make a cell cancerous1. The stochastic nature of the disease manifests in the form of both inter- and intra-tumor heterogeneity2,3. Inter-tumor heterogeneity refers to the existence of distinct mutational patterns in different tumors originating from the same patient, while intra-tumor heterogeneity refers to the coexistence of multiple cancer cell clones within a single tumor mass. Tumor heterogeneity especially contributes as a challenge in the early phase of drug development, where preclinical models with little to no patient relevance are used to identify, validate, and develop clinical candidates3.
The lack of preclinical models that capture cancer biology
While pre-clinical studies in conventional models such as cell lines and xenografts are a useful tool to screen compounds and provide useful biological insights, they do not show a good correlation with efficacy in Phase II trials or survival advantage in Phase III trials4
While cell lines are fast and easy to establish, they are markedly deficient in representing original tumor biology. While patient-derived xenografts and explants are better representatives of patient tumor antigen expression, they do not recapitulate the stromal component of the tumor, leaving open-ended questions on how the drug might respond in the tumor microenvironment.
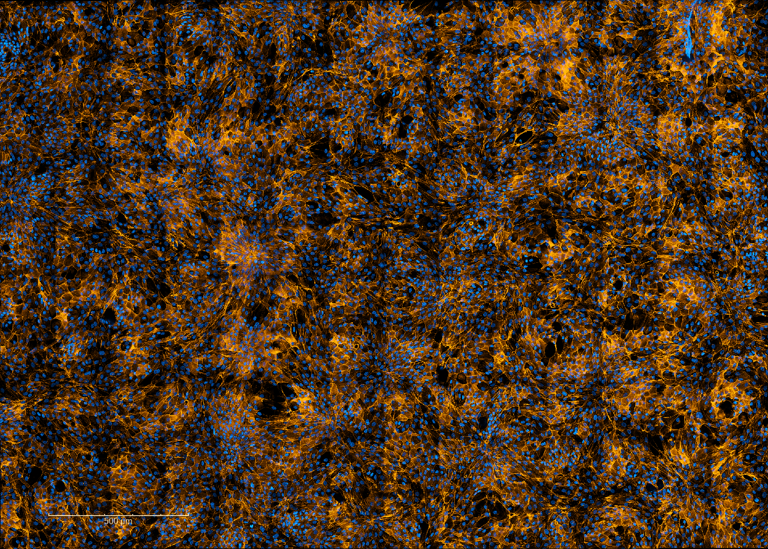
Mini tumors in the lab
HUB Organoids derived from patient-derived tumor samples or biopsies reflect crucial features in terms of tumor architecture, genetic makeup, and the composition of differentiated cell types. Tumor organoids show a remarkable representation of interpatient tumor heterogeneity5 and have shown promising data in predicting patient drug response in the lab6.
In a recent study7, HUB Organoids derived from colorectal cancer patients were used to develop the first bispecific against cancer stem cells in all solid tumor types. Remarkably, the bispecific was developed within five years, thanks to validating the therapeutic potential of the agent in a diverse panel of patient-derived organoids representative of the clinical setting.
Patient-derived organoids established from single cells in tumor-adjacent normal crypts also allow testing for off-target and off-tumor toxicities within the same patients, making it easier to cross out compounds with toxic effects early in the drug development pipeline.
Creating tumor organoid biobanks for personalized medicine
Through years of experience, the culture conditions have undergone optimization and expansion, facilitating the establishment of organoid biobanks of a diverse range of solid tumor types, including intestine, colon, bladder, lung, liver, ovary, pancreas, kidney, breast, and stomach.
Most biobanking studies confirm that patient-derived organoids (PDOs) reflect the characteristics of the primary tumor, at least at the level of bulk tumor DNA sequence8. Moreover, studies also show that the clonal drift over prolonged culture times for organoids is relatively small as compared to conventional models9,10.
Retrospective studies have indicated that the response of PDO to therapies closely resembles the initial response of patients to the same treatments11. Beyond the empiric potential of PDOs to help choose therapies for individual patients, large panels of PDOs representing one type of cancer have been used to develop biomarkers predictive of drug response12.
The evolution of organoid modeling is happening at an unprecedented pace, and the potential for this cutting-edge approach to revolutionize oncology and advance clinical research is truly exciting.
Want to know how patient-derived organoids can help you de-risk your drug development program? Book a free consultation with an expert.


.jpg)
.jpg)